It’s no secret that psilocybin and other psychedelics have had some impressive therapeutic effects in recent years. But what about mixing these medicines with antibiotics? Can psychedelic drugs safely interact with common antibiotics, or would this put users at risk for dangerous side effects? We know there are potential risks associated with taking any kind of medication, so it’s important to understand the relationship between psychedelics and antibiotics before mixing them. This especially applies to the growing community of psilonauts who are deciding to self-medicate as the expected prices for psychedelic-assisted therapy appear to be only affordable for those with deep pockets. In this blog post, we’ll take a look at the available research to explore if you can combine psychedelics and antibiotics – and how this impacts your health.
Limited research has made it difficult to fully understand the possible interactions between antibiotics and psychedelics. However, it is worth noting that specific types of psychotropic drugs have been known to interact with certain antibiotics, leading to the possibility that psychedelics could be affected in a similar way. Meanwhile, for the sake of this article, we will mainly examine case studies that involve people who have combined psychedelics and antibiotics and some resulting adverse effects.
[ez-toc]
Join our FREE Psychedelics for Beginners Course!

What are Antibiotics?
Antibiotics are a medication that can kill or prevent the growth of bacteria in the body, and are often used to treat bacterial infections.
There are three ways to take antibiotics: orally (by mouth) using pills, capsules, or liquids; topically using creams, sprays, or ointments applied to the skin or eye/ear drops; and injection or intravenous (IV) for serious infections.
Antibiotics side effects
Antibiotics can cause a range of side effects, which vary in severity. Some common side effects include:
- Nausea
- Rash
- Diarrhea
- Yeast infections
- C. diff infections, which cause diarrhea that can lead to severe colon damage and sometimes even death
- Severe and life-threatening allergic reactions
- Antibiotic resistance infections
What are psychotropic drugs?
Psychotropic drugs are a type of medication that impact the brain and have the ability to change one’s mood, behavior, and perception.
Psychotropic substances, or psychoactive substances, include alcohol, caffeine, nicotine, marijuana, antidepressants, anti-anxiety medications, stimulants, antipsychotics, mood stabilizers and certain pain medicines. Schedule l psychedelic substances like psilocybin, LSD, DMT, MDMA and other amphetamines are also classified as psychotropic substances.
Interactions between antibiotics and psychedelics
Antibiotics and psychotropic drugs can interact in several ways. One example is that some antibiotics may affect how the body processes certain psychotropic drugs, leading to potentially harmful side effects due to higher drug levels in the body.
The US National Institutes of Health (NIH) published a paper titled “Pharmacologic interactions of antibiotics and psychotropic drugs“, which explores potential interactions between antibiotics and psychotropic drugs. According to the paper, antibiotics and psychotropic drugs have various types and specific mechanisms of action and side effects. This can make drug interactions between them intricate and subject to variation depending on the specific drugs involved.
Liver Damage
Taking antibiotics and psychedelics at the same time can be harmful to the liver. Although rare, antibiotics can lead to liver damage or failure, while psychotropic drugs can raise levels of liver enzymes which could signal liver damage. Since the liver is responsible for breaking down drugs in the body, combining these two types of medication can increase the risk of liver damage or other adverse effects. In simpler terms, because both of these substances are metabolized by enzymes in the liver, taking them at the same time can exceed the liver’s capacity to process them.
Erythromycin and clarithromycin
Erythromycin and clarithromycin are antibiotics that can affect the liver enzymes that break down drugs like MDMA and LSD (1). This causes the levels of these drugs in the bloodstream to rise, increasing the risk of liver damage. In 2019, a study called “Cytochrome P450 (CYP) mediated metabolism of MDMA and its implications for MDMA-induced liver injury” was published in the journal Toxicology and Applied Pharmacology. The study examined the impact of MDMA on the liver and how it is metabolized by cytochrome P450 (CYP) enzymes in the liver. According to the study, erythromycin and clarithromycin can block CYP enzymes that metabolize MDMA, causing higher levels of the drug in the bloodstream and potentially raising the risk of liver damage.
Rifampin and isoniazid
Additionally, it seems like using certain antibiotics like rifampin and isoniazid can also harm the liver. This can happen even if they are taken alone. When taken with psychedelic drugs, the risk of liver damage may be greater. A study titled “Isoniazid and Rifampicin Induced Liver Failure: A Case Report” published in the Journal of Clinical and Diagnostic Research in 2017 had some interesting findings (2). The case report discusses a patient who suffered from liver failure while being treated for tuberculosis with isoniazid and rifampicin antibiotics and emphasizes the potential harm these antibiotics can cause to the liver. Although the report does not focus on the impact of these drugs on psychedelic substances, it does demonstrate the risk of liver damage when these antibiotics are used alongside other substances such as psychedelics.
While using psychedelics or antibiotics as prescribed by a healthcare professional, the risk of liver damage is usually low for most individuals. However, if someone combines these medicines, it could that risk increases. Liver harm risk is more significant for individuals with pre-existing liver conditions or those taking high doses of these substances however, anyone such medications should be mindful of the potential adverse reactions they may exhibit.
Toxicity
Some evidence shows that taking certain antibiotics may impact the way the body processes psychedelic drugs, which could result in high toxicity levels. A case report titled “Drug interactions with monoamine oxidase inhibitors: Ayahuasca, lysergic acid diethylamide, and mescaline” was published in the Journal of Clinical Psychopharmacology(1). The report documented a patient who suffered from severe toxicity as a result of taking ayahuasca while undergoing treatment with the antibiotic linezolid. According to the authors, linezolid might have prevented the enzymes that break down ayahuasca from functioning properly. This could have caused the drug to accumulate in the body and result in toxicity.
It’s important to note that there is limited data available on the potential risks and benefits of combining antibiotics and psychedelic drugs. This highlights a gap in research that needs to be addressed. It’s also important to remember that drug interactions can be complicated and may differ depending on an individual’s genetics and overall health. Hence, it is crucial to consult with a healthcare provider before combining various medications or drugs.
Examples of antibiotics that you should potentially not mix with psychedelics
Taking certain antibiotics can impact how the body processes psychotropic drugs. Due to this, there may be elevated levels of the drugs in the body which can increase the chances of toxicity.
Linezolid
Linezolid, also known as Zyvox, is a type of antimicrobial drug used to treat infections caused by gram-positive bacteria. It is approved for the treatment of bacterial pneumonia, skin and skin structure infections, and infections caused by VRE bacteria, which includes infections complicated by bacteremia. The antibiotic is a type of monoamine oxidase inhibitor (MAOI). This means it can interact with drugs that affect the levels of neurotransmitters in the brain, particularly with psychedelics such as LSD, psilocybin, and MDMA, which affect serotonin levels. Such interactions may increase the risk of serotonin syndrome, which is a potentially life-threatening condition.
Erythromycin

Erythromycin is an antibiotic frequently prescribed for respiratory tract infections. It’s used to treat illnesses caused by bacteria. These can include lung infections like bronchitis, pneumonia and Legionnaires’ disease; throat infection diphtheria; STD including syphilis; and ear, intestine, gynecological, urinary tract and skin infections. It also helps prevent rheumatic fever coming back. Erythromycin has the potential to interfere with the metabolism of specific psychotropic drugs, such as diazepam (Valium) and alprazolam (Xanax), as well as tricyclic antidepressants such as amitriptyline. This interaction may result in elevated levels of these drugs in the body, causing side effects such as sedation, drowsiness, and others.
Clarithromycin

Clarithromycin is a type of antibiotic that is prescribed for chest infections like pneumonia, skin problems like cellulitis, and ear infections. In addition, it is also prescribed to treat Helicobacter pylori, a bacterium that can lead to stomach ulcers. Like erythromycin, the antibiotic can impact the liver enzymes responsible for metabolizing drugs such as MDMA and LSD.
Rifampin & Isoniazid
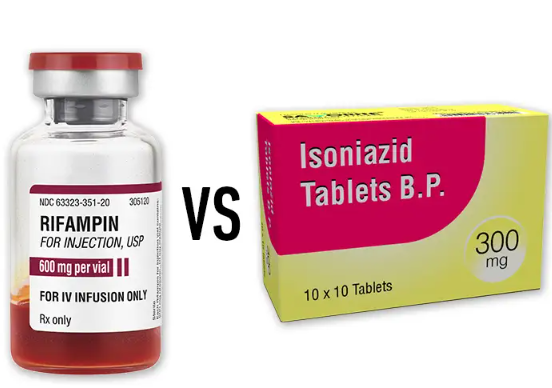
Rifampin and isoniazid are antibiotics that, when combined, they are used to treat tuberculosis (TB). TB is a severe infection that primarily targets the lungs but can also affect other parts of the body. Rifampin is also used to treat individuals with Neisseria meningitidis infections in their noses or throats, a bacterial strain that can lead to meningitis. As stated above, there are reports of liver damage when these antibiotics are used alongside psychedelics.
So, can you mix psychedelics and antibiotics? To be clear, it is risky to use psychedelics while taking antibiotics. If you want to try a psychedelic-assisted treatment and you are currently on antibiotics, it is better to wait until you have fully recovered before using them. Before use, it’s important to talk to a healthcare provider or an expert in psychedelic medicine to discuss any possible harm and ensure safe and responsible use.
References:
- Li, X., Yu, Q., Xu, Y., Zhang, M., Li, L., Li, X., … & Liu, Z. (2019). Cytochrome P450 (CYP) mediated metabolism of MDMA and its implications for MDMA-induced liver injury. Toxicology and Applied Pharmacology, 382, 114747.
- Sood, A., Midha, V., & Mahajan, R. (2017). Isoniazid and rifampicin induced liver failure: a case report. Journal of clinical and diagnostic research: JCDR, 11(4), OD09–OD10. doi:10.7860/JCDR/2017/23425.9587
- Barbosa, P. C., & Giglio, J. S. (2005). Ayahuasca, lysergic acid diethylamide, and mescaline: Drug interactions with monoamine oxidase inhibitors. Journal of Clinical Psychopharmacology, 25(6), 520-523. doi: 10.1097/01.jcp.0000180025.94790.0c.