
Another day, another study proving the efficacy of psilocybin to treat depression.
Last Thursday, the American Medical Association published on JAMA Network the results of a randomized, 6-week clinical trial involving 104 participants to evaluate a single-dose treatment for major depressive disorder (MDD). A 25-mg dose of synthetic psilocybin was administered to a total of 51 of those participants with psychological support, while the rest of the patients received a placebo with the same psychological support.
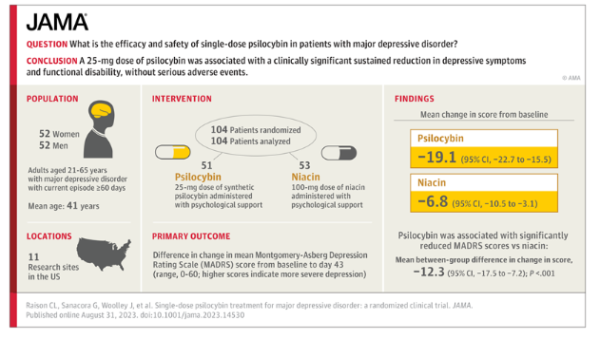
“Psilocybin administered with psychological support was associated with a rapid and sustained antidepressant effect, measured as change in depressive symptom scores, compared with active placebo. No serious treatment-emergent adverse events occurred,” the study found, with authors concluding, “These findings add to increasing evidence that psilocybin—when administered with psychological support—may hold promise as a novel intervention for MDD.”
Though the results of this study are familiar, it was actually quite unique in the realm of psychedelic research, being the first large, FDA-type, phase 2b study of psilocybin, with a bigger sample size than previous studies, as well as broadening scope from treatment-resistant depression disorder to less severe major depressive disorder.
Although psilocybin remains illegal in the vast majority of the United States, lead study author Charles L. Raison, MD, explained on a JAMA Network podcast that a single dose of the psychedelic can benefit the “many, many people [who] do not get adequate response to the antidepressants we have currently.”
“More than half of the people that are struggling with depression do not get a remission with currently available agents, and when they get it, they tend to lose it,” Raison said.
He continued:
“Something like psilocybin, which produces a long-term antidepressant response after a single treatment may be a different way of approaching it. You give it early in the course of the disorder, people then have this sort of change in their affective state that allows them to perhaps move through life without having to take an antidepressant every day and perhaps avoiding that situation where people end up with longterm, chronic antidepressant use.”
Following 6-8 hours of psychological preparation work and the actual 6-8 hour dosage experience, behavioral outcome assessments were completed a day after, a week later, two weeks later, four weeks later and six weeks later. “The six weeks post-dosing was the primary endpoint of the study,” Raison said. “And the primary outcome was change in depression symptom score as measured by the Montgomery-Asberg Depression Rating Scale, which is pretty much the standard thing done in the field.”
The study results reflect the anecdotal experiences shared by individuals who have used psilocybin to treat their depression. Retired firefighter Joe McKay, who was among the 9/11 first responders and suffered the post-traumatic stress from the ordeal for over a decade, recently described psilocybin therapy as “transformative.”
“I stopped taking the cocktail of pills I had been prescribed, many of which caused damaging side effects and were addictive,” he wrote in a guest column for CalMatters. “It’s not an exaggeration to say that psilocybin gave me my life back. It’s been transformative, and allowed me to feel happiness and joy in a way I never thought I would again.”





