
In the realm of psychedelic substances, one particular compound stands out for its potential to transform lives and challenge conventional notions of addiction treatment and personal growth. Ibogaine, derived from the root bark of the Tabernanthe iboga shrub, has captured the attention of researchers, clinicians, and individuals seeking alternative paths to healing. With its rich history rooted in traditional African spiritual practices, ibogaine has emerged as a substance with remarkable properties and profound effects on the human mind and psyche.
Ibogaine’s unique pharmacology and its intricate interactions with the brain have sparked intrigue and curiosity within the scientific community. This article aims to provide a comprehensive exploration of ibogaine, shedding light on its pharmacological mechanisms, potential therapeutic applications, benefits, risks, and the ethical considerations surrounding its use.
What Is Ibogaine?
Ibogaine, a naturally occurring psychoactive compound found in the root bark of the plant family of Apocynaceae such as Tabernanthe iboga. Ibogaine has garnered significant attention for its potential therapeutic effects on addiction and its use in spiritual and personal growth practices. This powerful substance has a long history of traditional use in African spiritual rituals, where it is revered for its ability to induce profound visionary experiences. In recent years, ibogaine has gained recognition in the Western world as a potential treatment for addiction, particularly in cases of opioid dependence. Despite its promising effects, ibogaine remains a controversial substance due to its potential risks and legal restrictions in many countries.
Ibogaine has a long history of traditional use in African spiritual practices, particularly among the Bwiti people of Gabon. It has been used for centuries in initiation rituals, healing ceremonies, and as a tool for spiritual exploration. In the 1960s, ibogaine gained attention in the Western world as a potential treatment for addiction, primarily due to the work of Howard Lotsof, who accidentally discovered its anti-addictive properties when he was 19 and addicted to heroin. In the 1980s, ibogaine was manufactured in capsule form and underwent successful trials in the Netherlands. In the 1990s, ibogaine left Europe and made its way to the Americas where Eric Taub and Lex Kogan systematized the treatment of ibogaine with centers across the world, with Deborah Mash conducting further academic research and clinical trials. Since then, ibogaine has been the subject of various studies and anecdotal reports, but research on its therapeutic applications has been rather limited.
Ibogaine Mechanism of Action
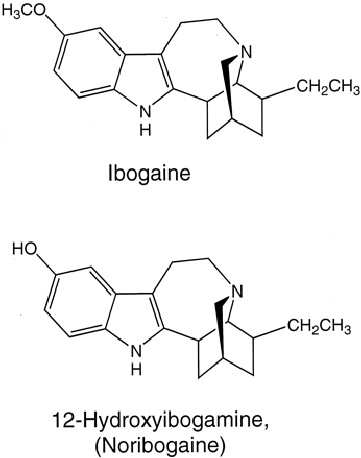
When ingested, ibogaine metabolizes into noribogaine, which interacts with various receptors in the brain, leading to a wide range of effects. At a molecular level, ibogaine acts on various neurotransmitter systems, including serotonin, dopamine, and glutamate receptors all at the same time. One of its primary targets is the opioid system, crucial in addiction and pain regulation. Noribogaine has been found to be most potent as a serotonin reuptake inhibitor, but acts as a kappa-opioid receptor agonist and as a weak µ-opioid receptor agonist, as well. Ibogaine binds to and modulates the activity of opioid receptors, altering the release and reuptake of neurotransmitters. This modulation is believed to contribute to the reduction of withdrawal symptoms and cravings observed in individuals undergoing ibogaine therapy for opioid addiction.
It has been found that ibogaine’s action at the kappa-opioid receptor is likely to contribute to its psychoactive effects, while weak agonist action on the 5-HT2A receptor contributes to its hallucinogenic effects, similar to that of serotonergic psychedelics. Additionally, ibogaine has been shown to not only lower dopamine levels, but also enhance its breakdown. By decreasing dopamine levels, Ibogaine may also work in reversing the effects of opiates in gene expression by returning neuroreceptors to a pre-addiction state. Addictive loops and pathways in the brain are reversed by ibogaine, which makes it a potential addiction treatment.
A 2006 research paper looking into the mechanisms of action of ibogaine suggested that it also binds to N-methyl-D-aspartate (NMDA), sigma-2 and nicotinic receptors. The authors propose that the binding at NMDA receptors contributes to ibogaine’s effects on opioid self-administration, the nicotinic antagonist action may mediate nicotine addiction, and sigma-2 action may mediate its neurotoxicity. The authors also found that a kappa-opioid receptor antagonist and an NMDA agonist partially reversed the effects of ibogaine, while an agonist and/or antagonist, respectively, increased some of its effects. This further elucidated the receptors at play in the mechanism of action of ibogaine.
What to Expect from an Ibogaine Experience?

The ibogaine experience is known for its intensity and duration. What a person will experience depends on the usual psychedelic factors, such as set, setting, dose, and method of consumption, so it can be hard to say what a person can expect when they take ibogaine. Users often describe a prolonged and immersive journey that can last up to 24 hours or more. The visionary experience of ibogaine is characterized by vivid and often intricate hallucinations, which can be both awe-inspiring and emotionally challenging. The ibogaine experience is known to be a bit unpleasant. Individuals may experience a sense of revisiting past memories, encountering symbolic representations, and gaining deep insights into their lives and behaviors. The introspective nature of the experience allows for profound self-reflection and the exploration of underlying psychological patterns.
The ibogaine experience can be broken down into three phases:
Phase 1
The first phase starts around 1 to 3 hours after consumption and can last 4 to 8 hours. This first phase has been described as being mostly visual with many users experiencing past memories during it. In the first hour, people can observe some physical discomfort, feeling heavy, dizzy and nauseated. However, after the first hour, the body adapts to the effects and according to anecdotal reports, individuals begin feeling from up to 95% of their opioid withdrawal symptoms. Some people may experience anxiety and fear as they face ego dissolution.
Phase 2
After this phase ends, the start of the second phase begins, which can last 8 to 20 hours. This is a most introspective phase where attention is directed at examining and evaluating the memories and experiences that were felt during the first phase of the trip. People report being easily agitated during this phase and prefer little stimuli as to not disturb their peace.
Phase 3
The last phase is a residual state that begins around 12 to 24 hours after consumption and can last up to 3 days. During this phase, psychoactive effects fade and users report a heightened sense of awareness and arousal, with some reporting a disruption in sleep patterns.
How Is the Ibogaine Experience Different Than Other Psychedelics?
While most classic psychedelics, such as psilocybin, LSD and DMT lead to externalized psychedelic experiences, ibogaine’s subjective effects are internalized and can last significantly longer than with other psychedelics. A classic psilocybin mushroom trip can last between 4 to 6 hours, the DMT experience has an overall time span of 15 minutes, the total duration of an LSD trip can go between 8 and 12 hours, and the ibogaine trip can last between 24 and 36 hours. Moreover, according to Tom Feegel, the Founder and CEO of Beond, a combination between a luxury retreat, a medical facility and wellness center that treats some of the hardest cases of addiction and trauma, compared the other psychedelics which can lead to complete dissociation of reality, those who enter an ibogaine are easily aware of what reality is. He explained that people in deep ibogaine states can simply rub the tips of their fingers to become aware of where they are and what they are doing. The psychedelic effects are experienced with closed eyes. This means that individuals can have lucid conversations when they open their eyes without experiencing visual hallucinations.
Although classic psychedelics and ibogaine can lead to ego death, the subjective effects from externalized psychedelic experiences can include individuals can travel to other dimensions and interact with spirit guides, aliens, or machine elves. Some of the best examples of an external psychedelic experience are described by Rick Strassman. He was the first American researcher to receive government approval to study hallucinogens after a two-decade ban. Between the years of 1990-95, he administered roughly 400 doses of N,N-dimethyltryptamine (DMT) to nearly 60 patients at the General Clinical Research Center of the University of New Mexico Hospital. While recording the physiological effects of DMT, such as heart rate and blood pressure, he also described participants’ overwhelming religious experiences that he later reported in his book, DMT: The Spirit Molecule (and subsequent documentary film), in which over half of the volunteers claimed to have interacted with non-human beings, traveling through a DMT tunnel and having an outer body near death experience while under the influence of DMT.
In comparison, the ibogaine experience leads to a deep introspective state where individuals enter a profound phase of self-reflection and are capable of accessing past memories and relationships, and feel a sense of unity and interconnectedness. In an interview with Tom Feegel, the Founder and CEO of Beond, a combination between a luxury retreat, a medical facility and wellness center that treats some of the hardest cases of addiction and trauma, the ibogaine experience was compared to a more vivid regression therapy or watching a movie of one’s life. Individual can either recall memories in first person or see moments of their life as a bystander. One can describe it watching a movie of one’s life, and having the capacity to access repressed traumatic memories, and revisit the scenes as many times as you like. Although this may seem like an uncomfortable experience, it is not necessarily the case as by this time, participants have experienced ego dissolution. This means that they can revisit a very clear visual depiction of life events without fear, shame, or guild. It is during this self-reflection that emotional healing often begins.
Ibogaine Benefits & Potential Therapeutic Applications

The effects of ibogaine can vary widely from person to person and depend on factors such as dosage, individual physiology, and mindset. The primary benefit associated with ibogaine is its potential to interrupt addictive patterns and provide individuals with a fresh start in their recovery journey. It has shown promising results in treating opioid addiction, with some studies suggesting significantly reduced withdrawal symptoms and cravings. Research suggests that ibogaine may help reset the brain’s neurochemistry and reduce withdrawal symptoms, making it a potentially effective tool for treating addiction. Ibogaine therapy can offer a unique opportunity for individuals to confront and address the underlying emotional and psychological factors contributing to their addiction. Moreover, the profound and transformative experiences induced by ibogaine can also facilitate personal growth, self-discovery, and spiritual exploration.
Some of ibogaine’s benefits may include its ability to:
- Help break addictive patterns
- Treat opioid addiction
- Ameliorate withdrawal symptoms
- Enhance cognitive abilities
- Increase self-awareness
- Generate greater emotional understanding
Despite the relative lack of large-scale clinical trials, early research and anecdotal evidence have reported positive outcomes in treating opioid addiction with ibogaine. Some statistics suggest that a significant number of individuals who undergo ibogaine therapy experience reduced withdrawal symptoms, decreased cravings, and extended periods of abstinence from opioids. However, it is important to interpret these statistics with caution due to the limited sample sizes, variations in treatment protocols, and the challenges associated with long-term follow-up studies.
Beyond addiction treatment, ibogaine has been reported to enhance cognitive abilities and increase self-awareness. Users often describe improved clarity of thought, enhanced introspection, and a greater understanding of their emotions and behavioral patterns. Additionally, some individuals report a sense of interconnectedness with the world and a deeper appreciation for life.
Research on ibogaine’s therapeutic use is still relatively limited, but early studies and anecdotal evidence have reported positive outcomes. However, it is important to note that the success rates can vary depending on individual factors, treatment protocols, and ongoing support after the therapy. Further research and larger-scale clinical trials are needed to determine the optimal treatment protocols, identify potential contraindications, and better understand the long-term effects and sustainability of ibogaine therapy.
What Are the Side Effects of Ibogaine?

Ibogaine is considered to be generally safe, however it is not without risks. One of the main concerns is its impact on the cardiovascular system. Ibogaine has been shown to affect heart rhythm and cause long QT syndrome at higher doses by blocking hERG potassium channels. Long QT syndrome is a condition that affects the relaxing of the heart after a heartbeat, which increases the risk of an irregular heartbeat; this can result in fainting, seizures, or sudden death. Additionally, there have been reports of fatalities associated with ibogaine use.
A paper published in 2012 analyzed fatalities associated with ibogaine between 1990 and 2008 and found that nineteen individuals died within 1.5 – 75 hours after consumption. These deaths were not attributed to any neurotoxicity, but rather cardiovascular failure due to advanced preexisting medical comorbidities. Thus, people with heart conditions should abstain from taking ibogaine. Additionally, it is crucial that ibogaine therapy is administered under strict medical supervision in a controlled environment by experienced professionals who are well-versed in its potential risks, proper dosing, and necessary safety protocols. Prior medical screening and thorough assessment of the individual’s cardiovascular health are essential to mitigate risks.
Even with prior medical screening, there are reports of people dying after taking ibogaine. A paper estimated that 1 in 400 people who take ibogaine suffer a fatal reaction.
Aside from the aforementioned side effects, ibogaine can also adversely interact with certain food and medications. Reason being is due to ibogaine being metabolized by the cytochrome P450 complex, which is an important superfamily of enzymes responsible in clearing compounds from the body. Due to ibogaine being partly metabolized by cytochrome P450, users must avoid foods or drugs that interfere with these enzymes, with specific focus on CYP2D6. A common example of foods that interfere with CYP450 are those containing bergamottin or bergamot oil, such as grapefruit juice.
Paroxetine, commonly sold under the brand name Paxil, has been shown to slow down the liver from breaking down ibogaine, thus increasing its side effects due to a systemic accumulation. People taking anticholinergic drugs may find that ibogaine decreases the effects of these drugs. Additionally, various medications used for glaucoma and Alzheimer’s increase the levels of acetylcholine, along with ibogaine, thus increasing the chance of side effects. Mixing QT-interval prolonging drugs with ibogaine can lead to serious heart issues. A full list of drug interactions can be found here.
A recap of side effects:
- Cardiovascular issues
- Long QT Syndrome
- Arrythmia
- Interactions with certain medications
- Interactions with certain foods
- Death
- Irregular heartbeat
- Low blood pressure
- Seizures
- Paralysis
- Difficulty breathing
- Heart attack
Can Ibogaine Cause Death and How to Prevent It?
Yes. However, it is important to note that, according to MAPS (Multidisciplinary Association for Psychedelic Studies), deaths associated with ibogaine occurred outside of medically supervised environments. Due to the potential health risks, ibogaine should not be administered without medical supervision.
Reputable treatment centers take steps to ensure patient safety, such as:
- Conducting medical screenings prior to treatment
- Cleansing patients of contraindicative drugs and substances before ibogaine administration
- Monitoring electrolytes and heart rhythms during treatment
- Having medical staff on hand or the means to transport patients to a medical facility in the event of an emergency
Using Ibogaine for Personal Growth

Beyond its potential therapeutic applications, ibogaine has gained popularity as a catalyst for personal growth, emotional healing, and spiritual exploration. The intense and introspective nature of the ibogaine experience allows individuals to delve deep into their subconscious and confront unresolved issues, traumas, and patterns of behavior. Many users report gaining profound insights into their lives and a heightened self-awareness that extends beyond the immediate effects of the substance.
The visionary nature of the ibogaine experience often involves vivid and symbolic imagery that can be interpreted as representations of one’s inner world. This can facilitate emotional and trauma healing and provide individuals with a unique opportunity for self-reflection, self-acceptance, and personal transformation. Some users describe a sense of spiritual connection, a deepened understanding of their place in the universe, and a renewed sense of purpose and meaning in life. It is important to approach ibogaine as a tool for personal growth with respect, preparation, and integration practices to fully benefit from its potential insights and transformative effects. As aforementioned, ibogaine runs severe risks, so its use must be solely done under professional guidance.
Ibogaine’s Legal Status
The legal status of ibogaine varies across countries and jurisdictions. In some nations, ibogaine is classified as a controlled substance due to its hallucinogenic properties and potential for abuse. In such cases, its possession, distribution, and use may be prohibited or strictly regulated. However, other countries have adopted more permissive regulations or consider ibogaine a scheduled medicine for addiction treatment purposes. It is essential to thoroughly research and understand the legal implications and regulations surrounding ibogaine in your specific country or region before considering its use. Engaging in ibogaine therapy in countries where it is illegal or unregulated can have serious legal consequences.
In the United States, ibogaine can be used within the city of Oakland, CA, after their city council voted in 2019 to decriminalize all entheogenic plants. Outside of the United States, ibogaine is legal to possess and distribute in Mexico, Costa Rica, Brazil, South Africa, Gabon, New Zealand, and the Netherlands, with treatment centers existing in most of these countries.
Myths Surrounding Ibogaine
Several myths surround ibogaine, and it is important to debunk them to provide accurate information to individuals considering its use. One common myth is that ibogaine can instantly and permanently cure addiction after a single session. While ibogaine can be a valuable tool in addiction treatment, it is not a magic bullet. Successful outcomes depend on a variety of factors, including the individual’s commitment to their recovery, ongoing support, and appropriate aftercare. Ibogaine therapy should be seen as part of a comprehensive treatment plan rather than a standalone solution. Ibogaine is considered an addiction “interrupter,” rather than a cure. This means that it eliminates cravings and withdrawal symptoms, which makes the road to recovery easier, but this does not inherently cure the addiction.
Another myth is that ibogaine is universally safe for everyone. While ibogaine has shown therapeutic potential, it carries inherent risks, particularly cardiovascular complications. Individuals with certain pre-existing medical conditions, such as heart conditions or liver problems, may be at higher risk when using ibogaine. Proper medical screening and a thorough assessment of an individual’s health history are crucial to ensure their safety during ibogaine therapy.
Additionally, it is important to dispel the misconception that ibogaine is a recreational drug. Ibogaine is a powerful substance with potent psychoactive effects, and its use should be approached with caution and respect. It is not intended for recreational purposes and should only be used under the guidance of experienced professionals in appropriate settings.
Conclusion
Remember, if you are considering ibogaine therapy, it is crucial to consult with qualified professionals and practitioners who can provide appropriate guidance, support, and medical supervision throughout the process. The decision to use ibogaine should be based on thorough research, informed consent, and a comprehensive understanding of the potential benefits and risks. While it has shown promise in treating addiction, it also carries certain risks for vulnerable populations. Ibogaine is not like other psychedelic drugs that can often be used recreationally, thus proper care must be taken before consuming it.
Ibogaine Frequently Asked Questions
What does ibogaine do to the brain?
Ibogaine affects a variety of neurochemical pathways. It blocks the nicotinic acetylcholine receptors and inhibits the release of catecholamines that are induced by substances such as nicotine, cocaine, and morphine. Ibogaine also inhibits the NMDA receptors. stimulates the opioid receptors, and increases levels of neurotensin. Ibogaine also interacts with the σ1 and σ2 receptors, voltage-gates Na+ channels, and Ca2+ channels. According to literature, noribogaine is a full agonist at µ receptors.
What are the side effects of ibogaine?
The side effects of ibogaine include nausea and vomiting, low blood pressure, cardiovascular issues, long QT Syndrome, arrhythmia, contraindications with certain drugs and foods, seizures, paralysis, feeling of heaviness, difficulty breathing, heart attack, and death. This is why it is critical to have ibogaine administered by medical professionals.
What are the subjective effects of ibogaine?
The subjective effects of the ibogaine include accessing repressed memories, experiencing ego dissolution, having vivid, introspective psychedelic journeys and altered perceptions of time. The ibogaine experience can last 24 hours with some even reporting a 36 hour trip, where individuals report emotional and psychological insights allowing them to deal with past or repressed trauma. In terms of physical effects, some individuals experience low blood pressure, minor motor impairments, nausea and vomiting. During the first stage of the ibogaine experience, people can feel anxiety and fear as they face ego dissolution.
What is the half life of ibogaine?
According to rat studies, ibogaine is processed mostly in the liver. After an ingestion of oral doses between 500 and 1000mg, ibogaine’s highest blood concentration is detected at approximately 2 hours. Approximately 90% of ibogaine leaved the body within 24 hours and it’s half-life is between 4 to 7 hours.
Is ibogaine FDA approved?
No. Due to it’s illegal status in the United states, ibogaine has not gone through the clinical trial system a drug needs to undergo for FDA approval. However, the DEA continues to increase ibogaine quota production for research purposes, and several decriminalization movements in cities in the unites States, such as California and Massachusetts have decriminalized ibogaine along with other natural psychedelics. Ibogaine is also included in Senator Scott Wiener’s proposed California psychedelic decriminalization initiative SB 58.
Does ibogaine lower blood pressure?
Yes. Ibogaine can decrease heart rate and blood pressure.
Is Ibogaine Used for Addiction?
Yes. In places where ibogaine is unregulated, such as in Mexico, ibogaine retreats and clinical centers are administering ibogaine to eliminate substance use, chemical addiction, trauma, depression, PTSD, and other mental health illnesses. A 2016 systematic review of animal studies demonstrated that ibogaine reduced addiction to cocaine, ethanol and opioids.
DISCLAIMER: Psychedelic Spotlight does not in any way encourage or condone the use, purchase, sale or transfer of any illegal substances, nor do we encourage or condone partaking in any unlawful activities. We support a harm reduction approach for the purpose of education and promoting individual and public safety. If you are choosing to use psychedelic substances, please do so responsibly.





